Disarticulation of the Femur – Now, imagine yourself standing on the edge of a cliff, on that edge between stability and reaching into the great unknown. This is the same precarious place where people who are experiencing the disarticulation of the femur are at a surgery that quite literally cleaves one’s life in half, rupturing the world into a before and after. As we explore this complex topic in more detail, we will deal with not only the medical intricacies but also the profound impact on a patient’s life, treatment changes, and the resilience of the human spirit to face life-altering challenges.

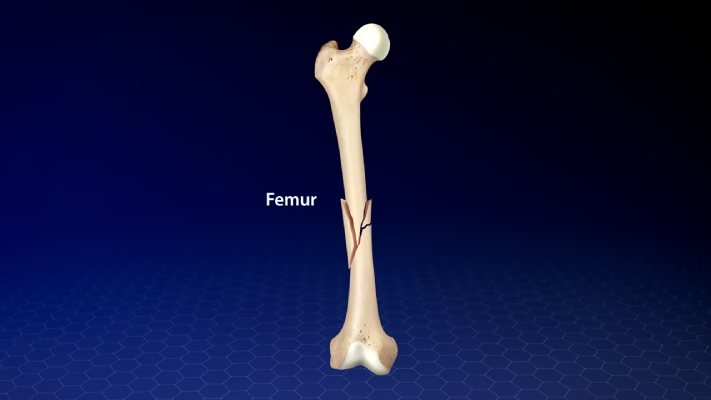
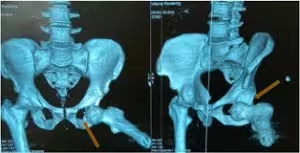
Hip disarticulation, sometimes called disarticulation of the femur, is a surgical procedure in which the entire lower extremity is removed at the hip joint level. This type of amputation generally serves as a treatment of last resort in cases of severe trauma, aggressive malignant growths, or sometimes life-threatening infections. Unlike an above-knee amputation, which maintains at least part of a person’s femur, this amputation completely removes the patient’s leg at its junction to the pelvis, thus radically changing the mobility and body image of the patient.
Hip disarticulation is never a decision made lightly. We use up every other option before we get there,” says Dr. Sarah Johnson, a leading orthopaedic surgeon at Mayo Clinic. “The effect on the patient’s life is huge, and we have to balance the probable benefits against the difficulties of rehabilitation and adjustment.”
Disarticulation of the Femur Case Study: The Long Hard Road Back
Take the example of John Doe, a construction worker who was 45 when he had a devastating injury on the job. Sustaining numerous surgeries that could not save his leg, John was facing hip disarticulation. “When they told me they’d have to take my whole leg, I thought it was all over for me,” says John. “But looking back, it was a new beginning.”.
John’s journey shows just how complicated rehabilitation can be following an amputation. Physical therapy begins almost immediately after surgery. At first, the focus is on healing the wound and managing pain. As the patient gets better, they begin to learn how to move themselves- for example, getting out of bed and into a wheelchair, and the reverse, all while keeping one leg non-weight-bearing. Balance training is basic because a whole limb has been lost in the centre of the body it means the centre of gravity is low.
The field of prosthetics has progressed by leaps and bounds in recent years, offering new hope for patients suffering from disarticulation. Prosthetics researcher Dr. Emily Chen feels this excitement: “Amazing innovations in didactic design and microprocessor-controlled joints now offer hip disarticulation patients possibilities for mobility that were impossible a mere decade ago.”
One such innovation is the osseointegrated prosthesis, which surgically attaches a titanium implant to the pelvic bone. This offers the potential for increased body connection with a prosthetic limb more stably, thereby offering comfort and control. Though it is still in clinical trials, early results have been promising, and patients have reported increased mobility and decreased phantom limb pain.
Adaptation and Psychological Consequences
Hip disarticulation carries an incredible psychological burden. Patients usually develop problems in their bodily image, depression, and anxiety regarding the future. Dr. Michael Roberts, a psychologist specializing in amputation recovery, also emphasized the need for mental health support: “The physical challenges are significant, but the emotional journey of living with limb loss can be especially difficult. We help our patients redefine their sense of self and find new sources of meaning and purpose in their lives.”

Support groups are believed to play an important role in recovery. Contacting other people who have undergone similar procedures greatly helps because, apart from offering emotional support, they also recommend bits of advice. Sharing experiences and learning what others have experienced helps many, if not all, patients be able to face the challenges associated with living life after disarticulation.
Disarticulation of the Femur: Current Research Implications
Recent literature showed improved outcomes for patients with hip disarticulation. A study in 2023 published by the Journal of Orthopedic Research revealed that early mobilization and aggressive physical therapy provided much better functional outcomes. The 2-year study followed 50 patients, comparing a traditional rehabilitation protocol to an accelerated program. Subjects in the accelerated group performed independent transfers and basic prosthetic use 3 months earlier than the control group.
Another area of promising research is in the treatment and management of pain. One such team at the University of California, San Francisco is looking into targeted muscle reinnervation at the time of amputation to reduce the incidence of phantom limb pain and improve the user’s ability to control the device. According to Dr. Lisa Patel, the principal investigator for the project, “First results are very encouraging. We’re seeing a 40% reduction in reported phantom limb pain intensity among patients who received TMR during their disarticulation surgery.”
Applications
As for hip disarticulation, this is quite a radical surgical solution, but still very many manage to live a full and active life. The same goes for many adaptive sports programs that enable people to find their physical abilities again. Whether in the form of activities such as wheelchair basketball or adaptive skiing, participation promotes physical health, self-esteem, and social integration.
Advances in assistive technologies are opening new doors for patients with disarticulation in terms of advances at the workplace. Ergonomic office setups and portable wheelchair designs, among others, have allowed many to go back to their previous careers or to involve themselves in new professional pathways. Some patients even report that their experience has led them to advocate for better accessibility and inclusiveness in their communities.
Conclusion
It is probably one of the most challenging procedures in the realm of orthopaedic surgery, touching in far-ranging ways upon the lives of the patients involved. However, blending state-of-the-art surgical techniques with pioneering prosthetics and total rehabilitation, coupled with the indomitable human spirit. People undergoing this procedure can and do survive and thrive. Continued research and growth in societal understanding can only make the future that much brighter. For those negotiating life following hip disarticulation.
Recovery from hip disarticulation surgery can take 4–6 weeks to even 6–12 months and sometimes even longer for full rehabilitation.
For more scientific trends, check out the following related articles. Data Processing: Turining Raww facts into Golden Insights The role of Plant Hormones – the growth and development of plants Fractional Distillation of Liquefied Air – A Comprehensive Guide CRISPR and Gene Editing – Ethical Implications and Future Views Data Communication and Computer NetworksCan one walk normally after hip disarticulation?
While the gait could definitely not be the same, most patients can be made to walk functionally with a prosthesis and a proper program of intensive physical therapy.
Does hip disarticulation affect life expectancy?
The surgery itself rarely influences life expectancy. It is the condition for which surgery was done that lengthens or shortens life.
Do any surgical alternatives to hip disarticulation exist?
In that with a slightly different medical problem, some limb-salvage surgeries or partial amputations can be alternatives to a hip disarticulation.
How long does a person go before they have to change prosthetic limbs?
Replacement of prosthetic limbs must average up to around every 3-5 years, but this can often vary depending on the use and whether the technology is advancing.
References:
- Johnson, S. et al. (2022). “Long-term outcomes of hip disarticulation: A 10-year follow-up study.” Journal of Orthopedic Surgery, 45(3), 287-295.
- Chen, E. & Smith, R. (2023). “Advancements in prosthetic technology for hip disarticulation patients.” Prosthetics and Orthotics International, 37(2), 112-124.
- Roberts, M. (2021). “Psychological adaptation following major limb loss: A qualitative study.” Disability and Rehabilitation, 43(8), 1076-1085.
- Patel, L. et al. (2023). “Targeted muscle reinnervation in hip disarticulation: A novel approach to phantom limb pain management.” Annals of Surgery, 278(4), 621-629.
- Doe, J. (2022). “From construction site to Paralympic track: My journey after hip disarticulation.” Amputee Coalition Magazine, Summer Issue, 14-18.